How the Opiate Conspiracy Widened
Part III in a series about the sociopathic push by big pharma to cash in on opiate production
Racket is pleased to be able to publish part III in a series about the opiate crisis by E.R. physician Matt Bivens (see his Substack, The 100 Days, here). You can read part one here, and part two here.
Many businesses will gleefully sell you a harmful addiction.
The tobacco industry was supposedly subdued decades ago by a historic legal beat-down, yet somehow spends $22 million every day promoting its wares. That’s nearly a million dollars an hour. Websites for kids sport vaping ads. “Cigfluencers” work the podcasts. And movies are smoke-choked like never before.
There was a time when a cigarette company could pay a mere $43,000 for Superman to be thrown into a Marlboro truck by the evil General Zod in front of Marlboro-smoker Lois Lane. (She had never smoked in the comic books, by the way.)
These days, modern Hollywood supposedly disdains tobacco cash. Yet somehow the movies remain one long, glamorous advertisement for cigarettes. Of this year’s ten Oscar Best Picture nominees, nine featured seductive and edgy smoking. (Only “Barbie” did not.)
The marketeers assure us we’ll be inhaling happiness and hipness. Maybe so, but there are also those hot, lung-damaging fumes — a reality that eventually catches up and kills about half a million of us every year.
(Brief digression: COVID-19 had a U.S. death toll of about 1.2 million over three tough years. Many COVID-19 victims were also smokers, so it’s hard to compare the pandemic and smoking death tolls. That said, we can certainly compare the public health responses. When COVID-19 arrived, we shut down the entire planet, and the virus would go on to kill an average of 400,000 Americans a year for three years. Smoking has been here all along — glamorized, marketed to kids — cheerfully killing 500,000 Americans a year, every year, forever.)
This series focuses on the Opioid Crisis, which has also killed hundreds of thousands and wrecked the lives of millions. But more people are killed each year by tobacco than by opioids — six times more. Smokers die 10 years younger on average than non-smokers, and even that understates it, because smokers don’t go out easily. Their later years are often needlessly miserable. In the emergency department, I see patients addicted to opioids, including many we have revived after life-threatening overdoses and some we have pronounced dead. But I see far more who have destroyed their lungs. I’ve known many of the longest-suffering smokers for years. They routinely arrive by ambulance struggling to breathe. And many, even those dependent on oxygen, still smoke.
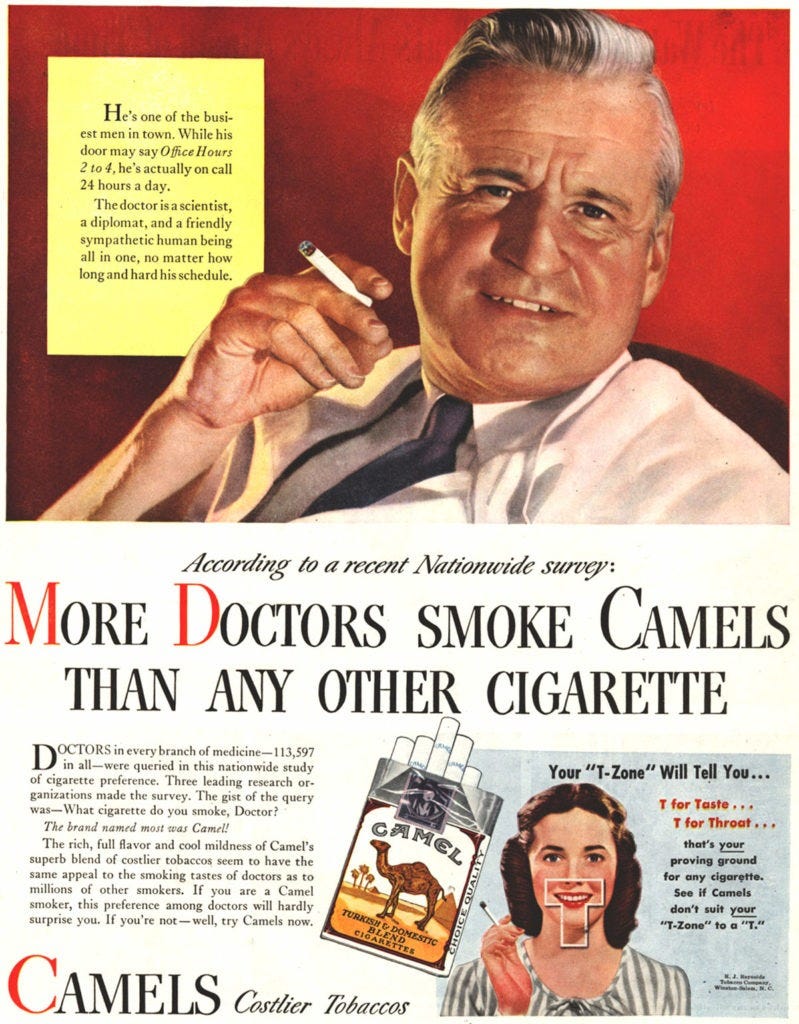
The tobacco industry has worked hard to cloud our collective understanding of their “product” — which is still the single greatest cause of avoidable mortality in America. They’ve done so via everything from those vintage ads that portrayed “doctors” lighting up, to the pseudoscience churned out by modern think tanks.
And yet, by comparison, the opioid industry remains a uniquely depressing case.
It is one thing for a profit-seeking corporation to sell ordinary people a frivolous activity — smoking cigarettes, binging alcohol, gorging on junk food — that is harmful. But the opioid manufacturers achieved an entirely new level of immorality. They used actual doctors to sell their wares — not a few avuncular, smoking actors in white coats, but tens of thousands of doctors and nurse practitioners. Opioids were not offered as a luxury item or a lifestyle choice, but as solemn and necessary medicine. This was a prescribed addiction. (In one study, four out of five people newly addicted to heroin started with a physician’s prescription.) And those who eagerly took cash to help sell this were not sleazy movie studios or soulless social media “influencers”, but the most trusted institutions of the House of Medicine.
Anatomy of a Long Con
First comes an idea: Tell doctors that the New England Journal of Medicine has discovered that opioids aren’t addictive. How? Easy. Cite a years-old, five-sentence letter to the editor called “Porter & Jick” (see Part II). The letter doesn’t actually say that, but the New England Journal’s archives also aren’t online before 2011, so for many years the busy, practicing physician won’t find it easy to double-check such claims. Spreadsheets from opioid manufacturers (again, see Part II) showed how methodically that fake literature base was generated. One pharmaceutical company made a spoof “Dr. Evil” motivational video for its staff inviting them all to laugh at how seriously doctors took these “studies”.
The next stage: Create trainings and seminars based on this fake literature base. Pay the leading institutions in medicine — including those that represent all doctors, license all doctors, and accredit all hospitals — to host said “trainings.” Force doctors and nurses to sit docilely in the audience, taking notes.
Every Respectable Source of Medical Education Was Corrupted
Doctors and nurses are expected to keep up with medical science. It’s an onus placed upon each individual, and it’s expensive. For example, I spent $579 this year subscribing to Emergency Medicine Abstracts (“We review over 600 medical journals each month so you don’t have to”) and an affiliated audio series called EM:RAP (Emergency Medicine Reviews and Perspectives). I also pay $500 a year to be a member of the Massachusetts Medical Society, which comes with a New England Journal of Medicine subscription. I read the monthly Emergency Medicine News, and I participate in hospital-based online and in-person trainings.
Some of this I do in a spirit of self-improvement. But I also need continuing medical education credits — CMEs — to stay licensed. How many credits, and on what topics, varies by medical specialty and from state to state. (The Federation of State Medical Boards has a summary page here.)
Everyone needs CME. We keep an eye out for it, and welcome it when it’s from a respectable source. So, if the American Medical Association — the epitome of button-down respectability — has a CME program, that’s got to be worth a listen, right?
Well, maybe not:

CME programs sponsored by the AMA about pain management were prepared by Purdue Pharma-paid physicians in 2003, 2007, 2010 and 2013. For much of this time, the OxyContin®-maker was also lavishing millions of dollars upon the AMA and its associated AMA Foundation, while Purdue’s President Richard Sackler was sitting on the AMA Foundation’s board of directors. Even as late as 2016, Purdue was still one of only two “Platinum Level” donors to the AMA Foundation.

Key context: Most of this is happening years and years after Purdue had already pled guilty (in 2007) to fraud and intentional deception aimed at creating a world of recklessly liberal opioid prescribing. Purdue admitted it did that, cut the government a check for about 5 percent, and then, as we will see, doubled down on even more egregious fraud and deception — some of that rolled out in these AMA courses.
What was the AMA, courtesy of opioid-funded marketing medical education, teaching us? Advil® and Motrin® are dangerous; opioids are safe.

State Medical Licensing Boards Are Bought Off
The AMA sounds like baseball, apple pie and patriotism. It’s the American Medical Association, all but wrapped in the flag. But in reality, it’s always been a money-focused lobbying group. (AMA did not respond to my questions). So, maybe it’s just an outlier? Surely one can trust the Federation of State Medical Boards, if that body chooses to publish guidelines and a 2007 book, Responsible Opioid Prescribing — proudly described as the “leading continuing medication education (CME) activity for prescribers of opioid medications.”
After all, if you don’t prescribe responsibly, it’s the state medical board that comes for you!
Yet opioid manufacturers also wrote most of this FSMB booklet. (The Wall Street Journal reports Purdue’s Dr. David Haddox was particularly active.) Companies including Cephalon, Endo and Purdue then paid the FSMB more than $250,000 to distribute 163,000 copies to physicians. For context, there are about 1 million licensed physicians nationwide — so that’s one booklet for every six physicians.
In fact, the FSMB was showered with more than $2 million in opioid cash over the next few years, while opioid manufacturer sales reps marched door to door, hand-delivering these booklets to doctors and nurse practitioners at primary care offices. The Mississippi lawsuit notes (paragraph 163, pg. 60) this was a powerful signal:
Drug companies relied on FSMB guidelines to convey the message that “undertreatment of pain” would result in official discipline … doctors, who used to believe that they would be disciplined if their patients became addicted to opioids, were [now being] taught that they would be punished instead if they failed to prescribe opioids.
Opioid manufacturers found Responsible Opioid Prescribing so business-friendly that they had their sales reps bring it to thousands of pharmacists, too. The New York attorney general’s lawsuit (paragraph 554, pg. 150) says the booklet:
taught that behaviors such as “requesting drugs by name,” “demanding or manipulative behavior,” seeing more than one doctor to obtain opioids, and hoarding, were not signs of addiction but were all really signs of “pseudoaddiction.”
“Pain” is Abruptly Declared a Vital Sign
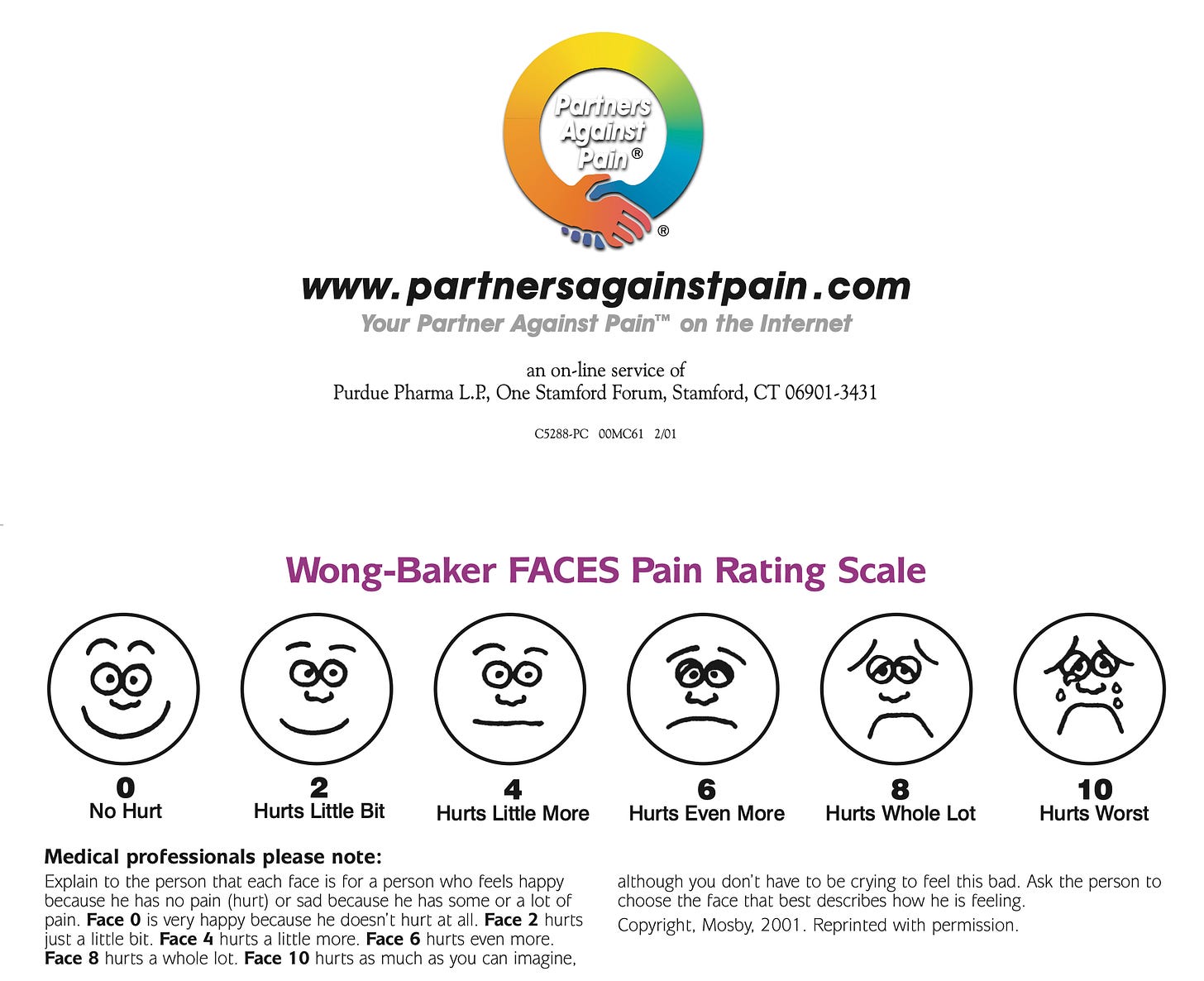
Enter the Joint Commission on Accrediting Healthcare Organizations, or JCAHO (pronounced JAY-Co). This non-profit used its enormous influence to insist, starting in 2001, that every hospital formally measure the pain of every patient.
It didn’t matter why the patient was there. It could be for a psychiatric crisis, or a pregnancy well-check. We still had to measure their pain. At the Joint Commission’s suggestion, many hospitals began to use 0-to-10 pain scale charts, examples of which can still be found sporting the Purdue logo:

What is the implication of being repeatedly asked, on a schedule, to focus all attention on your pain?
Imagine being asked out of nowhere to “rate your headache.” Surprised, you say, “Well, I don’t have a headache!” A little later, the nurse comes back, because it’s time to talk again about your headache. Do you think you might eventually feel a little headache coming on? If so, the good news is that we have a for-profit medication for that.
Some of us wryly suggested the Joint Commission ought to address constipation. It was under-assessed, undertreated, a national crisis! Every patient could report their bowel motility on a 0-to-10 scale, and we could medicate to a constipation score of zero. Life in the ER would be one long colonoscopy prep — but think of the MiraLax® revenues!
Never mind. The Joint Commission went further, and arbitrarily declared that the symptom known as “pain” was now a vital sign. It was to be checked regularly, right alongside the actual vital signs of blood pressure, respiratory rate, heart rate and temperature.

And it was not just every civilian hospital that would now consider “pain” a vital sign. The Department of Veterans Affairs simultaneously mandated this throughout military health institutions. Over at Purdue Pharma, Richard Sackler would make sure his company bought the rights to www.5thvitalsign.com. This was going to be gold for them.
The 100 Days is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
On a Scale from 0 to 10, How Much Do You Want Us to Care?
Patients asked to “rate their pain level” were supposed to understand a score of 10 as the worst pain they’d ever felt or could imagine:
Actually, though, patients almost always heard something else:
“On a scale of 0 to 10, how much do you want the nurse to pretend to care?”
Or:
“On a scale of 0 to 10, how frustrated and unhappy are you about being here?”
Some sort of “vital sign” number would emerge from this charade — and long-standing tradition holds that the doctor must address an abnormal vital sign. Nurses, prodded by Joint Commission-fearing hospital administrators, were poking doctors at regular intervals, and documenting things like: “MD aware of ongoing 7 of 10 pain, this RN awaits orders.”
The Joint Commission went further. It mandated posters on the walls in all patient care areas (including exam rooms and waiting rooms), which should declare: “All patients have a right to pain relief.”

These posters would become the ally of every addicted-to-OxyContin® person who ever faked a toothache. They would clutch their face and moan, and indignantly point at the wall.

Under Joint Commission pressure, “patient satisfaction” was surveyed, and physician groups could collectively lose money for low satisfaction scores. In a 2003 publication, the Joint Commission even warned doctors we could get in legal trouble for not giving enough drugs: “Recent court cases concerning patients with unrelieved pain,” the publication warned, show that doctors face “not only the investigation of the overprescription of opioids but increasingly the study of cases of underprescribing.”
Soon, the Joint Commission (it doesn’t go by JCAHO anymore) was hosting Purdue-designed and -financed CME trainings about it all:

So here we were. The national groups speaking for all doctors (the AMA), licensing all the doctors (the FSMB), and accrediting all of the hospitals (the Joint Commission), were reveling in opioid cash and singing to the same tune. They were providing doctors and nurses with mandatory “education”; forcing us to document that we were giving lots of opioids; warning us we could get in legal or other trouble if the patient reported not getting enough pain control.
The Emergency Department learns to loathe the Joint Commission
It was in this era that emergency departments came to solidify our deep and abiding hatred of the Joint Commission. We already loathed the occasional site visits. Middle managers — terrified that the hospital might somehow lose the favor of medicine’s Death Star and be all but vaporized — would appear in the ED for the first time in months, or sometimes even years, to tell doctors we could not have a cup of coffee next to our computer because “the Joint Commission is coming!”
The Joint Commission thinks it is unfair we blame it for that, and indignantly denies that they try to police where the doctors or nurses eat or drink. They say they’re just enforcing federal government workplace safety rules — it’s not their fault, blame the Feds! Also, they elaborate helpfully, as long as no food or drink is near any “cabinets, shelves, counters” or “work surfaces” “where the potential for contamination” exists, everything should be fine!
I am not alone in having had my paper cup of coffee ceremonially thrown away for my own safety and because “the Joint Commission is coming!”
All of which is backstory to the nightmare now unleashed on EDs with the “pain is the 5th vital sign” campaign, and the wall posters about patients’ rights to drugs. People addicted to opioids began pouring angrily into the EDs. The posters on the hospital wall told them we doctors had to give them Oxys! We had to do it! Opioid manufacturers had also been running a national multimedia campaign — with radio and television ads, and patient-facing web pages — to educate the public about their “right” to pain treatment. Such “know your rights” campaigns sent even more opioid-hungry people charging furiously our way.
Many spooked doctors would oblige with a dose of intravenous hydromorphone, known to all by the Purdue Pharma brand-name Dilaudid®. It is a synthetic opioid, similar to fentanyl but as every ED nurse knows, even more euphoric. Many an addict has requested it by name. Despite the “studies” (Dr. Evil air quotes) that FSMB and others were boosting about the absurd “pseudoaddiction” concept, having someone scream in your face “Get me Dilaudid!” is probably a red flag for actual addiction.
Doctors who refused would have to mentally prepare beforehand for the angry and emotionally manipulative confrontations: “You’re a terrible doctor! You’re going to force me to go buy heroin to treat this pain! You are going to make me a heroin addict! I’m probably going to die from heroin because you won’t do your job!”
Over time, the cunning opioid-seekers would present more sympathetically, in apparent extremis — “My back! My back!” — and then, instead of imperious demands, they would, through gasps of pain, tell us this had happened before, and “the only thing that worked was a drug that begins with a D, it was called D-something.”
Across America, the patient asking for “the drug that begins with a D” is a known emergency medicine trope. As a medical student in Washington D.C., I once watched in horrified awe as a resident physician innocently named two dozen drugs that began with the letter D, pretending to try to figure out what the ever-more-frustrated patient wanted:
“Was it Diphenhydramine?”
“No.”
“Doxycycline?”
“Uh, No.”
“Darbepoetin?”
“No.”
“Dicyclomine! I bet it was Dicyclomine! No? Hmm. Diltiazem?”
“No!”
“Divalproate? Doxylamine? Dobutamine? Dulcolax? Digoxin? Dexmedetomidine? Duloxetine? Diflucan?”
On other occasions, when an ED team did not have the energy or bandwidth to manage a manipulative and threatening patient, they might pay him off to leave with a script for, say, 20 oxycodone tablets.
Over the years, as the overdose cases poured in and the death toll soared, the Joint Commission began to have second thoughts. The “right to pain relief” posters came down. Everyone tried to pretend that the “pain is a vital sign” campaign had never happened. ED doctors began to push back, and to criticize colleagues who’d negotiate with terrorists. In some places, new posters went up on the walls, declaring this was an “Oxy-Free ED” — warning patients up front not to expect to leave with an opioid prescription. (My physician group in Massachusetts tried to put such posters up in 2015, but the lawyers said we couldn’t.)
Either way, the new hard line — don’t expect to leave with an opioid prescription unless your shattered femur was sticking out of your thigh — corresponded with a relatively rapid disappearance of the manipulative, demanding opioid-seeker. They mostly stopped coming. At this same time, OxyContin® was reformulated to make it harder to grind up and inject; and CDC reports a second wave of the Opioid Crisis kicked off with the rise of heroin. Just as threatened, they all did go buy heroin instead:

The Joint Commission: Defiantly Contrite, Owning up to Nothing
Cities and towns enraged by the opioid crisis have sued the Joint Commission. (This non-profit brought in more than $250 million in 2022). It has issued halfhearted mea culpas. A few years ago, a top official there e-mailed CNN to agree that insistently telling doctors to stop with the “exaggerated” concerns about addiction “was an important contributor to inappropriate prescribing patterns for opioids and the subsequent opioid epidemic.” He went on to admit:
“The Joint Commission was one of the dozens of individual authors and organizations that developed educational materials for pain management that propagated this erroneous information.”
Two longer articles by the same Joint Commission leader, published in 2017 first in the Journal of the American Medical Association and then as a freestanding pamphlet, were more defiant. Crucially: Neither ever mentions that the Joint Commission took money from Purdue Pharma and others in return for letting opioid manufacturers design and run Joint Commission-branded “education”.
Of course not. Why go there? (When I asked the Joint Commission, a 501©3 charity, who paid them how much, they replied they “cannot comment on topics that are currently under legal review.”)
Instead, we are told the Joint Commission erred out of enthusiasm — it was swept up in “a bold attempt to address widespread undertreatment and underassessment of pain” — never mind that this was probably never a widespread problem in the first place, until opioid-makers started shrieking otherwise. (Again, the Joint Commission accredits hospitals. We are talking about people who show up in pain at the hospital. They have a kidney stone, or broke three ribs falling off of a ladder, and now they’re at the hospital for that. Not providing pain medication for these people would be like Starbucks not making coffees. So, how was it decided that their pain was not getting assessed or treated? By opioid manufacturers, that’s how.)
The Joint Commission states that, alas, it had to step forward: “Many doctors were afraid to prescribe opioids despite a widely-cited article suggesting that addiction was rare when opioids were used for short-term pain” — that widely-cited article being — incredibly — wait for it — yes — the by-then infamous Porter & Jick five-sentence letter to the editor.
It’s a nice demonstration of the intellectual fogginess of this world that the same author, in a list of “lessons learned”, concludes his same article by complaining about everyone else’s over-reliance on the flawed Porter & Jick letter — apparently forgetting he had just cited it above to justify bold action:

Next time, Part IV: Is there anyone in medicine who can’t be bought?
Part I: A deep dive into the sociopathy of the Opioid Crisis.
Part II: The conspiracy to game the medical literature.
Part III: The conspiracy widens.





“Every Respectable Source of Medical Education Was Corrupted” You would think someone would have learned their lesson after the opioid disaster, but woohoo! Here we go again with genital mutilation, another medical money maker.
I am a 61 yo anesthesiologist who saw this coming 30 years ago when we saw the push to treat pain as a 5th vital sign and to deemphasise the addictive nature of opioids. The government, pharmaceutical industry and our medical societies all share the culpability for the disaster we now face. And none will ever admit responsibility. Shameful.